This coming week, the online cancer hashtag communities will be celebrating. Why, you ask? We have two good reasons.
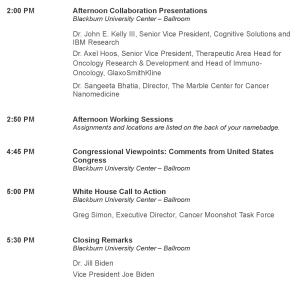
- The Cancer Moonshot Summit happens Wednesday, June 29, in DC and in satellite locations all over the US (see DC agenda at bottom of this post). While several of our members will be attending, we all have the opportunity to provide input to the Cancer Moonshot (deadline July 1).
- The 5th Anniversary of the beginning of Breast Cancer Social Media (#BCSM)—and the beginning of cancer hashtag communities on the web—happens July 4!
Our celebration will take the form of several coordinated chats open to everyone, regardless of cancer type.
Mon 6/27:
#BCSM Chat (use both #BCSM and #cancerchat hashtags) will host a cross-cancer chat at 9 PM Eastern Time about three of the Cancer Moonshot Working Group topics (check blog on #BCSM website for chat details):
–Expanding Clinical Trials
–Enhanced Data Sharing
–Precision Prevention and Early Detection
Ideas generated can be submitted online to the Cancer Moonshot.
Wed 6/29:
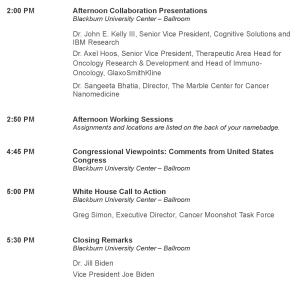
Cancer Moonshot events in DC and satellite locations (see agenda for DC Summit below)
Wed 6/29:
#Hcchat will conduct the official Moonshot chat (use both #Hcchat and #Moonshot hashtags) at noon Eastern Time on the topic “Will the Moonshot lead to the death of cancer?” This chat applies to all types of cancers. Special guest will be Vincent T. DeVita, Jr, MD, who was head of the NCI during Nixon’s Cancer Act and author of “The Death of Cancer.”
Thu 6/30:
#LCSM Chat (use both #LCSM and #cancerchat hashtags) will host a cross-cancer chat at 8 PM Eastern Time about the remaining four Cancer Moonshot Working Group topics (check blog on #LCSM Chat website for chat details):
–Cancer Immunology and Prevention
–Tumor Evolution and Progression
–Implementation Sciences
–Pediatric Cancer
Ideas generated can be submitted online to the Cancer Moonshot.
Thu 6/30:
Last day to submit Moonshot ideas at https://cancerresearchideas.cancer.gov/a/index
Sun 7/03:
#BTSM Chat (use both #BTSM and #cancerchat hashtags) will host a cross-cancer chat at 9 PM Eastern Time about our hopes and dreams for cancer research and treatment in the future.
Mon 7/04:
5th anniversary of #BCSM and cancer hashtag communities
Mon 7/04:
#BCSM anniversary celebration chat at 9 PM Eastern (use both #BCSM and #cancerchat hashtags)
The cancer hashtag communities hope you’ll join us for some (or ALL) of these special events and help us celebrate! To learn more about the cancer hashtag communities, visit http://www.symplur.com/healthcare-hashtags/ontology/cancer/
AGENDA FOR THE CANCER MOONSHOT SUMMIT IN WASHINGTON, DC